By Professor Jason Abbott – Medical Director – Endometriosis Australia
A hysteroscopy is a procedure where the inside of the uterus is examined through a thin telescope that is inserted through the cervix without the need for any surgical cuts to be made. The procedure may be performed in a clinic setting with mild discomfort and no general anaesthetic or it may be performed as a day procedure in a hospital under a local or general anaesthetic. The choice of where and how it is done will depend on equipment availability and the skillset of the doctors looking after you. Studies have shown that outpatient procedures are highly acceptable to women, since they do not need to have an aneasthetic and the discomfort is minimal with a rapid return to normal activities. If the procedure is performed in conjunction with a laparoscopy for endometriosis however, this would be done at the same time under a general anaesthetic.
Hysteroscopy may be used to both diagnose and treat specific conditions of the uterine cavity. Common problems that can be treated by hysteroscopy include:
- diagnosing and treating abnormal uterine bleeding
- investigation of infertility
- the treatment of scar tissue in the uterus (Asherman syndrome)
- removal of fibroids or polyps
- endometrial ablation (a treatment where the uterine lining is removed due to heavy periods)
- treatment of uterine abnormalities
For women having a procedure for endometriosis, it is not necessary to have a hysteroscopy as part of a treatment, although frequently there may be one of the above additional reasons to have a hysteroscopy. Scientific studies have previously investigated using a hysteroscopy and taking a biopsy of the endometrium to make a diagnosis of endometriosis, although this is not currently a method of diagnosing endometriosis and is not recommended for this purpose.
What happens during a hysteroscopy?
Prior to your hysteroscopy, you will be given specific instructions on any dietary requirements and this will depend on whether you are having an outpatient procedure, a general anaesthetic for the hysteroscopy alone or if you are having a laparoscopy for endometriosis in conjunction with your hysteroscopy.
Depending on where you are having your hysteroscopy will determine the pre-procedural process including the need for an IV line (drip), anaesthetics and monitoring equipment. For the procedure itself, hysteroscopy requires access to the vagina, cervix and uterus and you will have your legs placed in stirrups and drapes are placed over the lower part of your body. The cervix is then located either with the hysteroscope directly or using a speculum and held using a special holding clamp. The hysteroscope (the technical name for the thin telescope – about 2.5-5mm wide for diagnosis) is placed into the cervix and advanced whilst looking at a television screen where the image can be seen. The uterus itself is only a potential space, meaning that either fluid or gas is connected to the telescope and flows into the uterus to hold the walls apart so that the inside of the uterus can be seen. The telescope is advanced until the uterine cavity is entered and all the walls can be seen.
Any problems in the uterus may be noted and treated at the same time as they are seen. Special instruments may be used through a thin channel that is within the hysteroscope including fine scissors and graspers for additional surgeries that are necessary. These instruments help to take out abnormal tissue to be sent for pathological testing. For procedures done where you are awake and more extensive surgery needs to be undertaken, a general anaethetic may need to be organized.
Following a hysteroscopy, once you have fully recovered, your observations are stable, your bladder is working normally, any pain is controlled with oral medications and you can eat, drink and walk as normal you will be discharged home. You are likely to have some vaginal bleeding for a few days up to 2 weeks since there is often local bruising within the lining of the uterus from the procedure itself. Your period may also come at a time different than what you expect, but should come back to your normal cycle after this initial change.
Complications of hysteroscopy
Significant complications are very uncommon at the time of hysteroscopic surgery and serious complications occur in less than 1/2500 cases. That is for every 2500 hysteroscopies, there is less than one serious complication. Complications specific to hysteroscopic surgery include uterine perforation where a hole is made in the uterus. Usually this will have no significant consequences, although you may require an overnight stay for observation. It may also be necessary to do a laparoscopy to have a look at the outside of the uterus (if this was not being performed at the same time). Bleeding may be a consequence of this type of complication although it would be very rare to require a blood transfusion. If the hole was made with an instrument during a surgery where there was an abnormality being removed from the uterus (e.g. a fibroid or a polyp), then damage to other organs such as the bladder or bowel may result and this is a potentially serious complication. If this was to occur, further surgery such as either a laparoscopy or a laparotomy (a large incision made in the abdomen) to look for damage as a precaution since it is safer to treat any problem immediately then to have a consequence at a later time that needed treatment.
Other complications that may occur with hysteroscopy include the risk of fluid absorption into the bloodstream. During surgeries where there abnormalities such as fibroids are being removed, the absorption of too much fluid may lead to a salt imbalance in your bloodstream, which may cause wet lungs or rarely swelling of the brain. These are very serious complications and can be prevented by monitoring the amount of fluid lost during a hysteroscopic procedure.
You should not have a hysteroscopy if you are pregnant, since there is a risk of causing a miscarriage. You should inform your doctor if you think that you are pregnant and your procedure may be delayed. Your doctor will inform you if your surgery needs to be timed with your menstrual cycle or there are any other considerations.
Hysteroscopy and Endometriosis
For women who have suspected endometriosis and infertility, it is very common (and in fact sensible) that if there is to be a laparoscopy, then hysteroscopy be performed for assessment of the uterus, the cornua (the technical name for the entrance of the tubes into the uterus) and for a biopsy of the lining to look for any contribution to infertility in this area. For women who have suspected endometriosis and pain, often laparoscopy is performed as a surgical treatment and if there is no indication for looking inside the uterus by hysteroscopy, this is not necessary to improve the outcome of the procedure. Should your specific signs and symptoms suggest a problem with the uterus, then hysteroscopy may be recommended. You should discuss with your medial team if this is the right procedure for you.





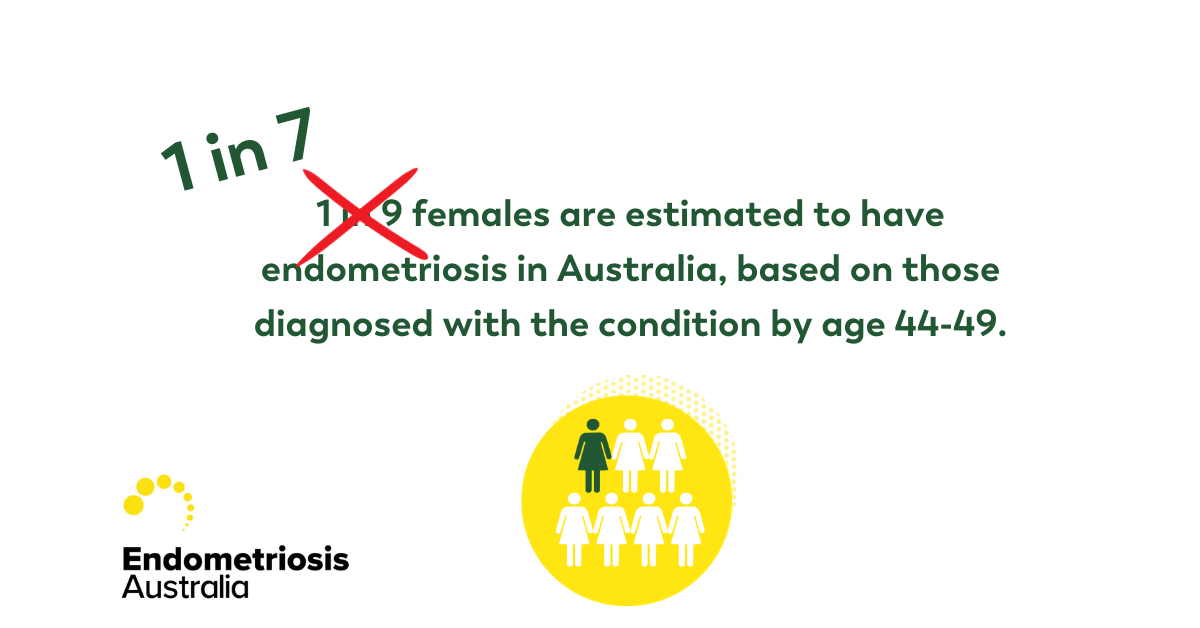
 ABOUT ENDOMETRIOSIS
ABOUT ENDOMETRIOSIS I HAVE ENDOMETRIOSIS
I HAVE ENDOMETRIOSIS SUPPORT US
SUPPORT US