By Professor Jason Abbott – Medical Director, Endometriosis Australia
Perhaps this title seems blatantly obvious to all women with endometriosis, however there is so much more to it than that, since menstruation and painful menstruation are inextricably linked to why there are so many issues with periods and pain and the diagnostic dilemmas of endometriosis.
When you think about it, pain is not usually a part of what we would consider ‘normal’ and yet menstruation is in fact a painful process. The nature of menstruation requires the release of a group of chemicals from the eicosanoid family – largely prostaglandins, but also other chemicals from this group – and these chemicals cause the blood vessels that extend to the outer layer of the endometrium to go into spasm and lead to menstruation. Easy. Except that it is not. It is well known that when you cut off blood supply to a tissue, that tissue then undergoes the process of ischaemia (no oxygen) and inflammation results. The by-products of inflammation are pain producing chemicals such as prostaglandins that regulate the ‘normal’ process of menstruation. And women do this month after month after month (except when they are pregnant or breast feeding – but I will get to that in a minute).
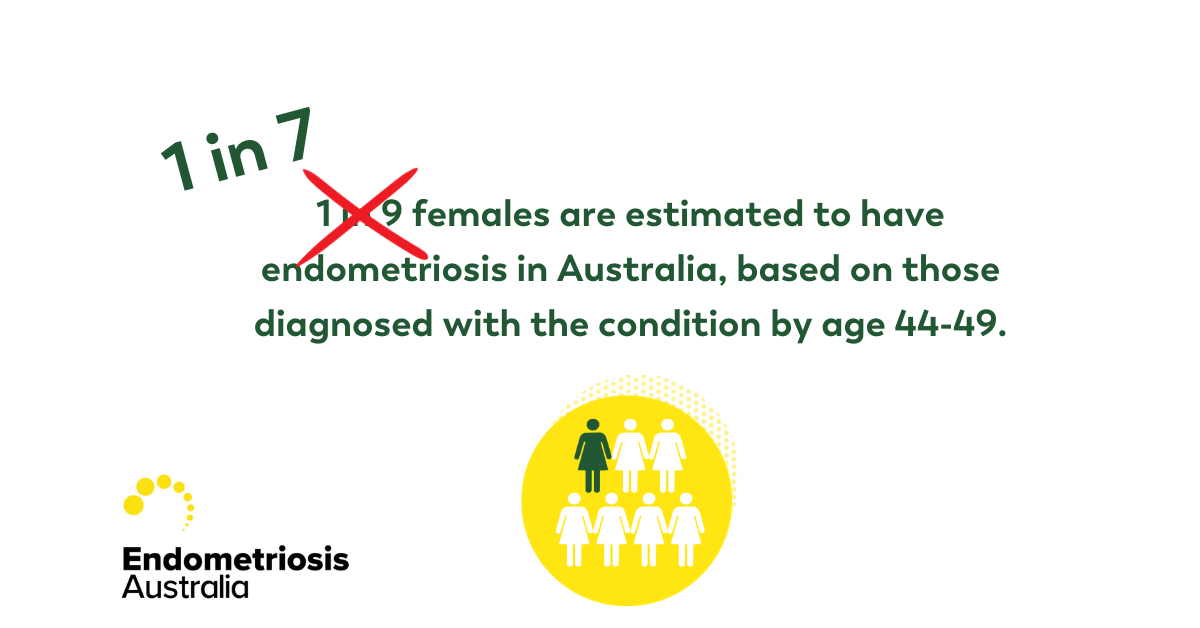
So how does this relate to endometriosis? Well, consider that if menstruation in all women releases these chemicals and we know that more than 95% of women have pain with some cycles during their lifetime and 50% of women have pain with each and every cycle and yet only 10% of women have endometriosis, then the diagnostic dilemma starts since the maths doesn’t add up – because we have both normal (the majority) and endometriosis sufferers (the minority) in this group. How do we tease out normal from abnormal and when does it cross that line from ‘normal’ pain to ‘abnormal’ pain? The answer is not exactly simple.
It is suggested that from the onset of symptoms to the presentation to a healthcare professional, women with endometriosis wait about 4 years. It may then be between 3-9 years before they have a diagnosis even after presenting to their health care professionals and the process of menstruation is part of that. Consider that if a man presented to his health care professional with cyclic pain for 3-5 days each month, you can bet that there would be a range of tests done immediately. That is not due to any sexist delineation, but purely because there is no part of male physiology that has pain as a normal part of homeostasis (the word used for the bodies regulatory systems to keep everything in balance and constant). Women on the other hand have pain in many parts of their homeostatic functions and all of them around reproduction – ovulation, menstruation and parturition (birthing) are all painful processes. And are therefore all normalised. So that is fine until normal is no longer normal and endometriosis sticks its ugly painful head in your pelvis.
So the delay in diagnosis is partly due to the fact that women often ignore their own symptoms (or they are told they are ‘normal’ by mothers, sisters, friends and health care professionals) – at least for a while. Clearly if there is pain, and that pain is due to inflammation from prostaglandins then medications such as anti inflammatories are very helpful, since they act on the pathway of inflammation and reduce that chemical load leading to less pain. These work in both ‘normal’ menstruation and in pain associated with endometriosis, but may be less effective for women with endo, simply because there is a greater load of these chemicals in the body. The caveat here is that if you are taking this type of medication and it is not controlling your symptoms to the point where you can get on with your life, then seek medical help and ask about the possibility of endometriosis. This is a much more likely diagnosis if there is a family history of endo – 7-8 times if you have a mother or sister with the disease.
So no cycles are the answer right? – well yes – at least in part. One of the mainstays of endometriosis management is to reduce cyclic variation and give a constant background of hormones, since it is the rise and fall of hormones and the shedding of endometrium with its elaboration of pain producing chemicals that contributes to the chronic pain that women with endometriosis suffer from. And early intervention when there are no changes to the nervous system that take women from acute pain to chronic pain is the way to go. I am often surprised that many women with menstrual pain – be it endometriosis associated or not “just put up with it” since they “don’t want to cover anything up”. There is no cover up – pain is painful and if you can reduce that and reduce your risk of chronic pain, then do so. We know that it is much harder when you already have chronic pain to get rid of it.
Painkillers alone are not going to prevent endometriosis growth, and neither will the pill or progesterones in any form – we know that too. But these are often a good start to reducing pain or reducing the cycles that lead to pain (through stopping ovulation and or menstruation and or the direct effects that progesterones have on endometriosis lesions). If these are not controlling symptoms and neither are all of the low-risk adjuvant treatments (exercise, diet, local heat, acupuncture etc.) then surgery may be considered. So, when done well and in expert hands, surgery will be able to make the diagnosis and remove the lesions, but it can’t change the underlying cause and this means that there is always the risk of pain recurrence – 50% risk of pain symptoms within 5 years and about a 30% chance of disease recurrence in that same time (note that recurrence of pain is not always associated with a recurrence of disease). But surgery carries risk as well as benefit and we have no scientific evidence that early removal improves pregnancy later in life (so prophylactic surgery is strongly discouraged – just as scheduled surgery should be discouraged – there is no benefit to ‘just having a quick look’ if you are an asymptomatic endometriosis sufferer).
Pregnancy does reduce the pain associated with endometriosis – at least temporarily – but this is since there is no cycle and very high progesterone levels. Once you have delivered and are no longer breast feeding, then cycles will return and often so too will the symptoms of endo return. So pregnancy is not a prescription and should not be considered as a treatment. Have your babies when you want, but do keep in mind that even with the very best help, egg age in the number one factor in pregnancy and fertility declines from the age of 30. Early and many pregnancies are recognised as protective for endometriosis (as it is for breast cancer, endometrial cancer, myomas and other gynaecological diseases) since the reduction in cycling is what will often drive many gynaecological disorders but it is not possible nor practical for the modern woman to be forever pregnant. So have your family if and when you want to, but keep in mind that fertility is not guaranteed in any woman.
So where does this leave the woman with endo? Well, there are a few simple considerations that may make life a little easier let’s step through a few:
- If you have period pain, then consider physical pain controls (water, exercise and diet – low response rate, but low risk) or over the counter preparations – anti-inflammatory medications or paracetamol (better response rate, but slightly higher risk as they do have side effects).
- If the pain continues consider hormonal suppression to regulate your cycle – the OCP and progesterone in any form may help – response rates are better, but side effects are also increased and these are not for every women. There is no age limit to these medications and teenagers and young girls could have endometriosis and at least consideration should be given to the diagnosis and careful planning and management undertaken.
- If hormonal suppression is not working or is not tolerated, surgery may be an option. If a woman wants a diagnosis, this remains the only option for her, but again the risks are higher since it is a surgical procedure. Making the diagnosis early is never a problem, since if there is endometriosis there, then putting a name to it will often help direct and guide treatment and whilst I have heard that making the diagnosis in young women is problematic since it means women are ‘labelled’, well if the disease is there, then she has endometriosis and she may be treated appropriately and if she doesn’t then we can consider alternative diagnoses and avenues for treatment. The analogy that I draw here is that if you consider the diagnosis of diabetes or even cancer in a young woman, then making that diagnosis early can considerably affect the way that treatment ensues (and the way that she is treated). The women herself is often relieved to know that there is some disease process and may contribute to her health improvement, and having a chronic disease is not uncommon and those with asthma, diabetes, or arthritis manage to live with their ‘label’ and often do better because their health care professionals go straight to the heart of their issues.
- Awareness and consideration that endometriosis may be the cause for the excess or non responsive period pain is important. This is where you and groups like Endometriosis Australia come in. So many women and so many health care professionals remain uneducated about endo. But it is getting better. In a recent publication in the Journal Human Reproduction a group from Melbourne reported that many Australian doctors knew about endometriosis, but often the advice given was conflicting or prioritised fertility issues over all else (quality of life or pain), so it appears that we are getting the message out there but more work needs to be done.
- Support each other and raise the profile of endo for the one in 10. Endometriosis Australia needs your support to continue this message. Join us on Saturday March 19th at one of our EndoMarch High Tea’s being held around the country. This is your opportunity to ‘End The Silence’ and start the conversation.
Professor Jason Abbott