By Dr Danny Chou – Endometriosis Australia’s Clinical Advisory Committee
Endometriosis occurring in and around the nerves are thankfully uncommon, particularly when it comes to involvement of major nerves such as the sciatic nerve. To discuss the condition of endometriosis in and around the nerves and see what can be done, lets look at a real-life case.
Case study
Miss AB is a healthy 24 year old lady who ceased the oral contraceptive pill whilst training for a half marathon and developed right hip and buttock pain, which became progressively worse over a short duration. Initially the pain occurred only during menstruation and ovulation but became more constant over the next 6 months with excruciating exacerbations during menstruation that rendered her housebound for 3 days of each month. She had no period pain or other pelvic pain to suggest endometriosis. She was taking strong painkillers to control the symptoms, but the pain still keep her awake at night. She could not sit for long or lie on her right side because of her right buttock pain. There was also pins and needles over the back of her right thigh, calf, heel and front of her foot. Miss AB walked with a limp because of her hip and buttock pain and noticed loss of muscle size over the upper aspect of her right buttock. She restarted the oral contraceptive pill but her symptoms did not improve. She had physiotherapy treatment and acupuncture to no avail.
Her family doctor organised multiple investigations including ultrasounds of her pelvis and right hip, X-rays of her right hip and lumbosacral spine as well as CT scans of her right hip and lumbosacral spine, which were all normal. Miss AB then saw an exercise physician who organised a magnetic resonance imaging (MRI) of her pelvis, which revealed a 3.5cm endometriotic lesion over the pelvic segment of her right sciatic nerve, thus arriving to the diagnosis of endometriosis over her right sciatic nerve. Her MRI also picked up wasting of her right gluteus medius and minimus muscles, which are signs of superior gluteal nerve injury. Miss AB was then referred to a gynaecologist specializing in endometriosis who also referred her for a comprehensive neurosurgical consultation.
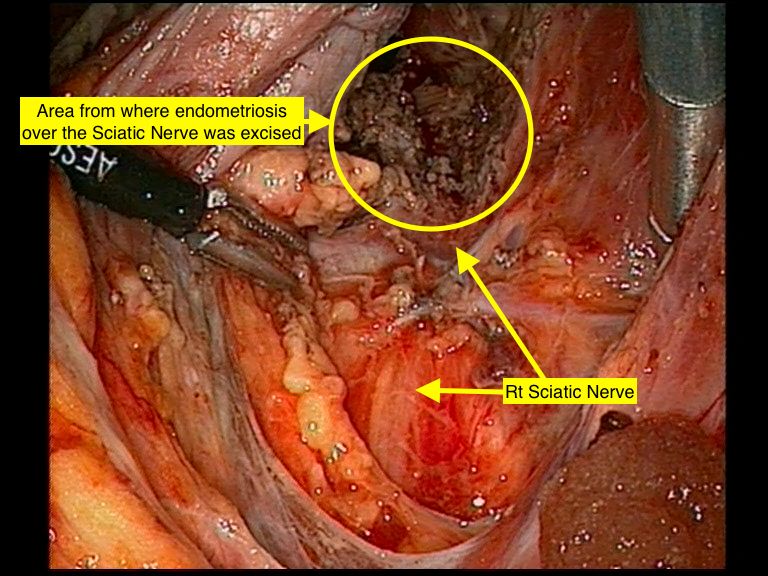
Following a multidisciplinary discussion involving a neurosurgeon, orthopedic surgeon, gynaecological oncologist and gynaecologist the patient underwent laparoscopic excision of endometriosis from the sciatic nerve. She had no disease in her pelvis. She recovered well from her surgery with significant improvement of her symptoms. Miss AB was followed up with hormonal treatment to minimise endometriosis recurrence until she was ready for family. Four years after her surgery, she is now is pregnant, with IVF assistance.
Fig 1. Right pelvic sidewall demonstrating Right Sciatic nerve and site where endometriosis was excised.
Symptoms of endometriosis involving pelvic nerves
Miss AB had a rare type of endometriosis where the only endometriosis she had was over her right sciatic nerve area, often referred as isolated endometriosis of the sciatic nerve (1), which can be very difficult to diagnose as it can present very much like a typical case of sciatica. More commonly, women with endometriosis involving nerves would also have endometriosis in the pelvis and therefore would have the typical endometriosis symptoms of period pain, pelvic pain and painful sex to alert the doctor that we are dealing with endometriosis and if there is nerve involvement and related symptoms one would think it is likely to be endometriosis related.
It is worth noting that there are 3 different types of endometriosis: 1) peritoneal endometriosis, 2) ovarian endometrioma and 3) deeply infiltrative endometriosis (DIE) and it is the deeply infiltrative endometriosis that can infiltrate into the bowel and bladder as well as in and around the nerve. Peritoneal endometriosis is the most common type of endometriosis and thankfully consists of only small superficial lesions over the peritoneum, which is the lining of the pelvic cavity. Nerves in the pelvis are located deep in the pelvis away from the peritoneum. Neurological structures that are closest to area of pelvis commonly involved with endometriosis are the hypogastric nerves and inferior hypogastric plexus, which is a meshwork of fine nerves, situated on the deep aspects of each pelvic sidewall. These structures are likely to be the most commonly involved nerve structures by endometriosis and they are autonomic nerves, which are responsible for visceral functions such as bladder, bowel and sexual function and operate at a subconscious level (that is they are not under our control like the motor nerves that control hand movement for instance). The often subtle effects from the involvement of these autonomic nerves by endometriosis may not be appreciated by either the woman or her medical team.
However when endometriosis infiltrates further afield and affects the deeper sacral plexus consisting, which are thicker networks of nerves coming out of large holes on the outer aspect of the sacral bone (the bottom part of the spinal cord) at the back of pelvis, more specific nerve related symptoms can be recognized. This may include pain and altered sensation along areas in the legs or parts of the pelvic region or muscle weakness and rarely even paralysis of muscle groups. When a major nerve such as the sciatic nerve is involved such as in Miss AB there can be the typical pain along the back of the leg with altered sensation in the same area. The commonest cause for sciatic pain is due to the nerve being compressed from a bulging vertebral disc between two segments of the spinal column. This is the more typical ‘sciatic pain’ and is associated with degeneration or trauma to a disc. This is quite different to Miss AB’s case of endometriosis growing into an area further away from the spinal cord and pushing on the sciatic nerve located in the pelvis. Thus accurate diagnosis is essential for correct treatment. In case of diagnostic uncertainty it is absolutely essential to have a comprehensive neurosurgical consultation. The most commonly affected somatic (as opposed to autonomic nerves) nerves by endometriosis are the sacral plexus and sciatic nerve (2). Other pelvic nerves that can be affected include obturator nerve, pudendal nerve, superior and inferior gluteal nerve.
Investigations
There is no specific blood test to diagnose endometriosis though Ca 125 could be suggestive. Pelvic ultrasound is the main gynaecological imaging modality and the ability now to diagnose deeply infiltrative endometriosis through specialist ultrasound has been a major advances in our diagnostic ability. Nerves in the pelvis are too small and too deep to be detected on ultrasound. CT will not be helpful either and even MRI may be normal unless there is large endometriotic nodule such as in the case of Miss AB. This creates some diagnostic dilemmas and in the case where there is no abnormality seen on imaging, treatment may be medical rather than surgical, since the surgical treatment is not without substantial risk.
Treatment
Apart from different analgesia for pain control, commonly used hormonal treatments for endometriosis in the form of oral contraceptive pill and different Progestogen (e.g. Provera, Primolut N) can be tried. Some improvement of neurological symptoms in case of suspected Isolated endometriosis would support the diagnosis. As in with Miss AB resumption of oral contraceptive pill did not help her symptoms and surgery is usually required.
Surgery for endometriosis should ideally be carried out laparoscopically. Severe endometriosis can be very challenging and special ultrasound looking for DIE which is likely to be present in cases of endometriosis involving the nerves, can be very helpful with surgery planning so that appropriate doctor carries out the laparoscopy for the expected level of difficulty. If during laparoscopy, more severed disease is encountered, the procedure may be abandoned or incomplete and repeat surgery will be required. Repeat surgery for incomplete surgery can be more difficult because of subsequent inflammation and scarring from initial surgery. If there is significant endometriotic involvement in other neighbouring organs multidisciplinary consultations and combined surgery would bring expertise from each specialty for best surgical outcome. Common specialists involved in multidisciplinary endometriosis surgery include colorectal surgeon and urologist to carry out surgery in the bowel or the urinary tract (bladder or ureter) as appropriate to her/his area of expertise. Whilst it is imperative that a patient with neurological symptoms has an expert neurosurgical consultation, a neurosurgeon will not perform laparoscopic procedure on pelvic nerves, as their expertise is in surgery in the brain and spinal cord and they do not perform laparoscopic surgery. Endometriosis, being a gynaecological condition and best understood by gynaecologist, endometriosis over pelvic nerve, by default, have been carried out by gynaecologist with special interest in endometriosis and complex gynaecological laparoscopic surgery. Surgery for endometriosis involving nerves requires a thorough understanding of the deeper nervous structures in the pelvis, located in an area that is not ventured in the practice of ordinary gynaecological surgery. Much knowledge of such conditions have been built by the pioneering work of Professor Marc Possover who established a new field of pelvic surgical specialty that specifically looks at conditions affecting pelvic nerves called Neuropelveology www.theison.org (3).
Miss AB’s laparoscopy confirmed a normal pelvic cavity with no endometriosis in her pelvis. However on exploration of deep lateral space over the site of Sciatic nerve revealed the 3.5cm endometriotic lesion with surrounding fibrosis overlying on top of her right sciatic nerve as could be seen on her MRI (Fig 1). In addition, there was also endometriosis encasing her right obturator nerve and surrounding tissue (Fig 2 &3). The obturator nerve supplies the muscles to the inner aspects of the thighs and causes the thighs to squeeze together (the movement is called adduction) and Miss AB had this weakness as a result of her endometriosis and imaging confirmed this and required surgery to this area in addition. Dissection of the disease from a nerve is very delicate and potentially risky surgery, since damage to the nerve may lead to temporary or permanent damage and loss of muscle and nerve function – so should only ever be undertaken by experts and only after consideration of alternatives and a full discussion of risks.
Treatment for Ms AB following surgery consisted of 6 months of Zoladex followed by Progestogen, as she was not able tolerate oral contraceptive pill due to side effects. Three years following her surgery and after trying for pregnancy naturally she decided for IVF and is now pregnant!!!!
Nerve endometriosis is a very rare form of endometriosis and its management is both technically difficult and requires a dedicated and expert team and should not be undertaken by those without specific training in this area.
Dr Danny Chou – Endometriosis Australia Committee
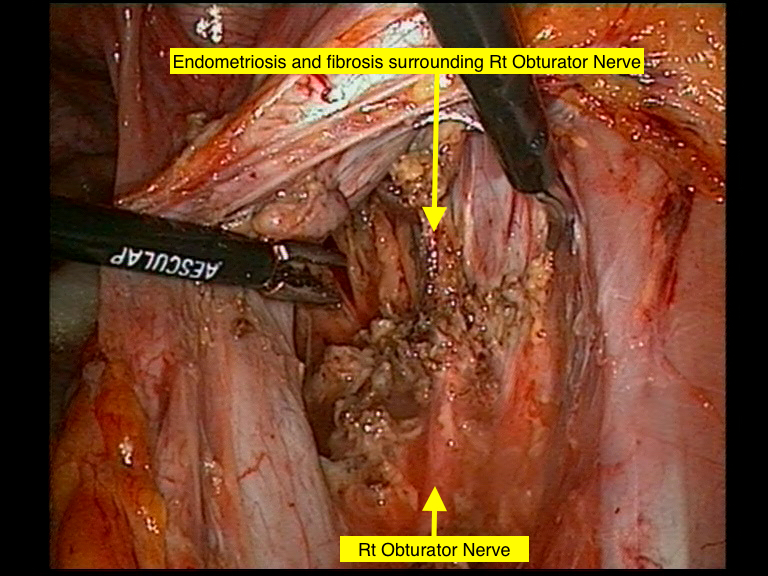
Fig 2. Right pelvic sidewall with Right Obturator Nerve encased with endometriosis
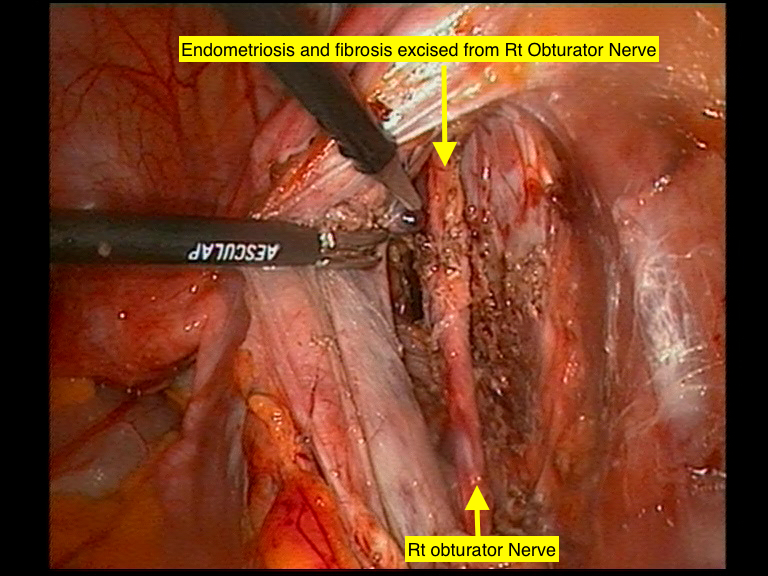
Fig 3. Right pelvic sidewall after having endometriosis excised from Right Obturator Nerve.
References
1. Possover M et al. Isolated infiltrative endometriosis of the sciatic nerve: a report of three patients. Fertil Steril. 2007 Feb; 87 (2): 417. E17-9
2. Possover M et al. Laparoscopic therapy for endometriosis and vascular entrapment of sacral plexus. Fertil Steril. 2011 Feb; 95 (2) 756-8
3. Possover M. Neuropelveology: New Groundbreaking Discipline in Medicine. Journal of Minimally Invasive Surgery. 2015; 22 (7): 1140-41