What is the connection between inflammation and the menstrual cycle? This article breaks it down.
What is the menstrual cycle?
The female reproductive organs (the organs used for having a baby) include:
- The vagina,
- The uterus (womb),
- The fallopian tubes (the tubes that the egg travel down).
Your menstrual cycle includes a rise and fall of hormones, changes in the reproductive organs and your period (if you don’t become pregnant).
Different things happen at different parts of the menstrual cycle. So, we often talk about what happens on certain days of the cycle. We start counting the days of your menstrual cycle from the first day of your period; this is ‘Day 1’.
There is a big range in what makes a ‘normal’ menstrual cycle. The time between periods is usually about 28 days. However, between 24-38 days is considered normal. The normal length of a period (the time you are bleeding) can be between 1 and 8 days. So don’t be concerned if your cycle is not the same as someone else’s. If you have any concerns, you should speak to a health professional.
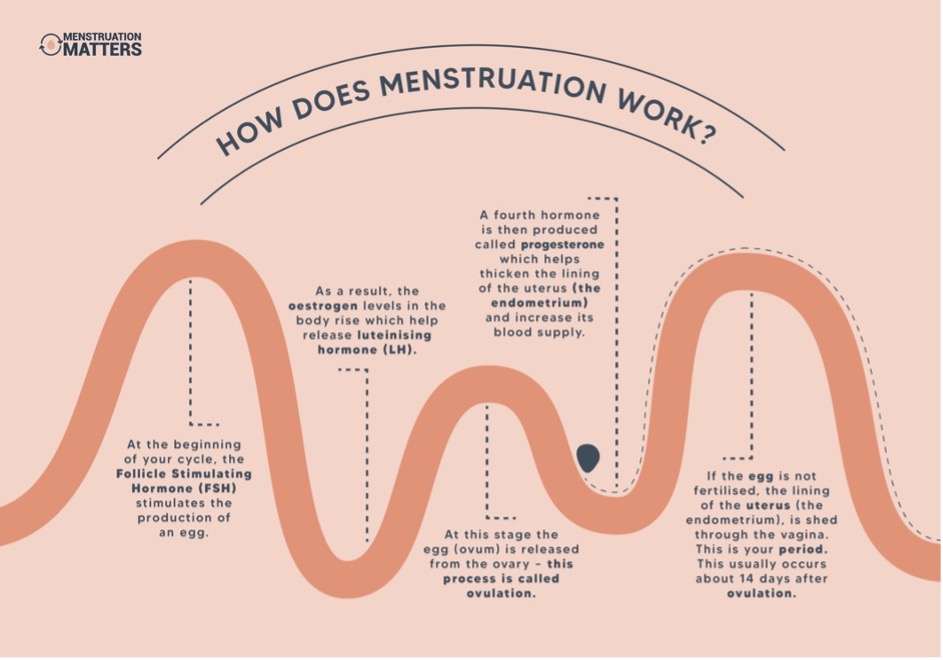
Four major hormones play a key role in producing and releasing the egg in preparation for pregnancy. These are (1) Follicle Stimulating Hormone (FSH), (2) luteinising hormone (LH), (3) oestrogen and (4) progesterone. The infographic below explains what each of these does during your menstrual cycle.
What causes inflammation?
So what does inflammation have to do with your menstrual cycle? Inflammation often leads to pain and is a major reason why periods can be painful.
If there is no pregnancy after the egg is released, progesterone levels fall. This fall in progesterone changes some of the fats that are in the walls of the cells that line your uterus. They first form a different product called arachidonic acid, and then make a type of hormone called prostaglandin.
These prostaglandins are released when your uterine lining breaks down during your period. Prostaglandins play a key role in how your body responds to inflammation.
There are a lot of other chemicals that also seem to affect the menstrual cycle. One of these is called Interleukin 6 (IL-6). Some studies have suggested that IL-6 levels in the blood are raised in people with endometriosis and the more IL-6 in your blood the more ‘severe’ the endometriosis is.
Recently however our research study found that IL-6 levels change a lot. It means these levels do not help diagnose endometriosis. Our research also showed that the levels of IL-6 didn’t seem to change even when pain and symptom scores were lower. This means we can’t use IL-6 to measure how severe your symptoms are.
How does inflammation cause menstrual symptoms?
These inflammatory chemicals can have powerful effects on the uterus. They cause the uterus to contract, and this reduces blood flow to the uterus. This is a bit like what happens in a heart attack. This results in painful cramps that many people get during their period. The levels of prostaglandins in the menstrual fluid change with time. When prostaglandin levels are low the cramps are less, and when they increase so does the severity of the cramps. Medications such as ibuprofen and mefenamic acid are commonly recommended to treat period pain, as they are non-steroidal anti-inflammatories (NSAIDs) and interrupt the pathways that cause prostaglandin production.
Prostaglandins aren’t just responsible for cramps. They can also make you more sensitive to pain. If that wasn’t annoying enough, they can be absorbed back into the body from your menstrual fluid and move around in the bloodstream. This can cause symptoms like headaches, nausea, vomiting and dizziness. They often cause more frequent contractions in your bowel, resulting in loose bowel motions, affectionately named ‘period poops’ by some. We know prostaglandins are responsible for these because when we use synthetic prostaglandins to bring on labour in pregnant women, we see the same symptoms.
Inflammation can affect more than just your period too. Cytokines are small proteins involved in many different processes including immune response and inflammation. If you have a lot of these cytokines in your blood before the period can cause some pre-menstrual symptoms especially changes in mood.
Written by,
Dr Mike Armour

