By Dr Michael Wynn-Williams – Endometriosis Australia’s Clinical Advisory Committee
Warning: Contains surgical imagery
Endometriosis of the urinary tract involves endometrial “like” glands and stroma in or around the bladder, ureters or kidneys. In up to 20-50% of people with pelvic endometriosis, it is found close to the bladder and ureters. Endometriosis that grows directly into the bladder muscle or ureter occurs less commonly in only about 1-6% of cases. The symptoms associated with urinary tract endometriosis can be relatively nonspecific, making diagnosis difficult.
The urinary tract is made up of the left and right kidneys, which connect down to the bladder in the pelvis by a long tube called the ureter (image 1). Each kidney is about the size of your clenched fist. They function as our blood filtration system to remove potentially harmful substances and waste through the formation of liquid urine. The urine travels from the kidneys down through each of the tubular ureters, where it is stored in the bladder, to be expelled at your convenience through the urethra. Endometriosis can have direct and indirect effects on all the anatomical structures in the pelvis and, as a result, cause a variety of symptoms.
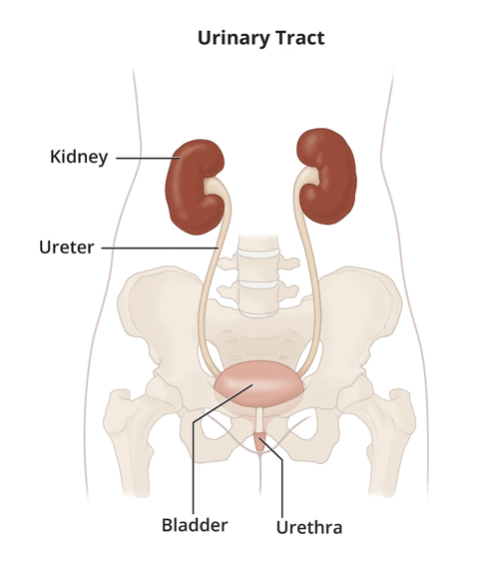
Image 1: The urinary tract, Kidneys, Ureters and Bladder
It is well recognised that one of the main symptoms of endometriosis is pelvic pain, which most commonly occurs before and/or during menstruation or at other times in the menstrual cycle. Many people experience a wide variety of symptoms related to endometriosis, which often relates to where the endometriosis is growing within or outside the pelvis. The most common site for endometriosis involving the urinary tract are lesions of superficial disease on the peritoneum, which is a thin layer that covers all the structures in the abdomen and pelvis, around the bladder. This form of endometriosis is not growing into the bladder muscle itself, but lies instead on the surface of the bladder, (Image 2). It may be difficult to differentiate the symptoms of this common form of endometriosis from other locations. People may experience pain with a full bladder or passing urine, or they may experience urinary frequency. These are all common symptoms of any pelvic endometriosis.
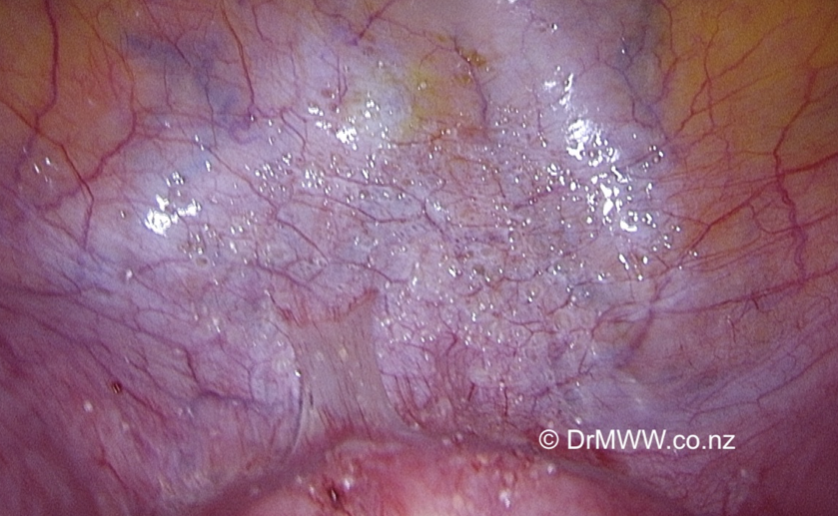
Image 2: Extensive superficial endometriosis over the bladder peritoneum
The next most common urinary tract endometriosis site is superficial lesions growing around the area where each of the ureters travels within the right and left sides of the pelvic walls before they enter into the bladder muscle. Again, in this situation, pain symptoms are often difficult to discern from other locations in the pelvis. The ureters travel close to the nerves that control the bladder, vagina and bowel, and endometriosis may affect their function in various ways.
The rarer but very significant type of disease we see is deep infiltrating endometriosis (DIE), affecting both the bladder and the ureter in different ways with different symptoms. Deep endometriosis in the bladder muscle wall can cause pelvic pain as the bladder fills or empties with urine. On rare occasions, blood can be seen discolouring the urine (haematuria) at the time of the period or found on a urine dipstick with your General Practitioner. Significant pelvic pain may be caused by deep infiltrating endometriosis growing around or in the wall of the ureters in the pelvis. The endometriosis may start to compress or constrict the ureter and affect the flow of urine from the kidneys. Urine can back up in the ureter and cause is to distend (hydroureter). This may also occur when endometriosis growing on enlarged ovaries starts compressing the ureters. As a result, urine starts to back up in the kidneys (hydronephrosis), potentially causing lateral back pain and ultimately permanent damage to the kidney. As we only have two kidneys, treatment must be swift to avoid long term health consequences such as raised blood pressure and eventually loss of kidney function. It is very rare for endometriosis to grow directly in the kidney, but it has been found growing around the kidneys and extending from the liver into the kidney.
Investigations for urinary tract endometriosis can be challenging. The majority of urinary tract endometriosis is made up of superficial peritoneal disease on the bladder or over the ureter and will not be seen on diagnostic transvaginal ultrasound or other investigations. Deep infiltrating endometriosis may now be seen with transvaginal ultrasound, when performed by experienced Sonographers, Radiologists or specially trained Gynaecologists / Endometriosis Surgeons. DIE can be seen growing in the bladder wall and around the ureters with good accuracy (Image 3). Magnetic Resonance Imaging (MRI) can also be useful in detecting urinary tract disease. It is important to remember that a negative ultrasound does not rule out the presence of endometriosis. Endometriosis in the bladder is also often found by Urologists when performing a cystoscopy (a surgical camera in the bladder) on people who present with blood in their urine. (Image 4 & 5)
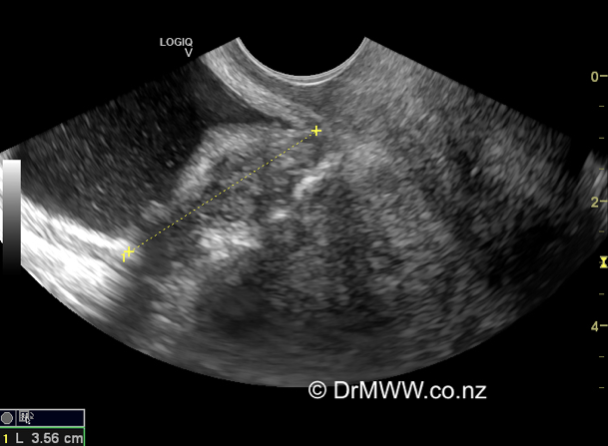
Image 3 -3cm Bladder deep infiltrating endometriosis (DIE) nodule seen on transvaginal ultrasound
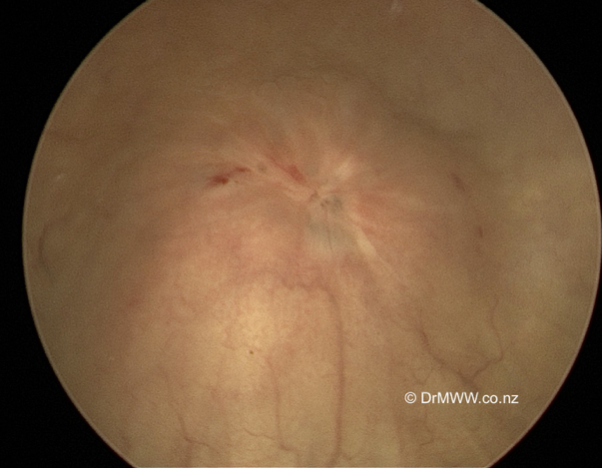
Image 4: Bladder DIE muscle lesion seen at cystoscopy
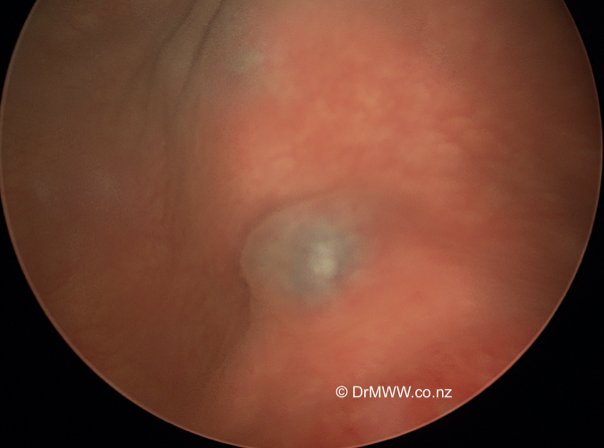
Image 5: Bladder muscle DIE lesion seen at cystoscopy, the blue areas represent endometriosis growing through the surface, causing haematuria (blood in the urine)
The doctor who ends up managing urinary tract endometriosis depends on the patient’s symptoms. Some people may have mild or no symptoms and can be managed by their general practitioner with simple hormonal treatments or anti-inflammatory medications. Unfortunately, we know that many people can have a wide range of symptoms that can affect some or all aspects of their lives, including education, work, relationships, sexual function and fertility. It is well reported that many people struggle to get a diagnosis of endometriosis from their GP’s or Specialists. We know the diagnostic delay from onset of symptoms to diagnosis of endometriosis varies from 6 to 12 years.
People can see a Gynaecologist who specialises in the field of endometriosis and who is appropriately trained in the diagnosis and management of urinary tract endometriosis. In Australia and New Zealand, these skills are acquired through the Australasian Gynaecological Endoscopy and Surgery Society (AGES) advanced laparoscopic fellowship program. This extra two-year program is completed after the RANZCOG six-year specialist training program. This training has been critical in producing knowledgeable and skilled specialists who can manage all stages of endometriosis. There are also many Gynaecologists who have gained significant experience in the management of endometriosis without attaining an AGES qualification. Endometriosis specialists will work in a multidisciplinary team with other specialists such as Urologists and Colorectal Surgeons. Urologists may be needed if a ureter is being compressed or blocked and requires decompression with a stent (a plastic straw placed in the ureter to allow the urine to flow). They may also be involved to assess how the ureter and kidney are functioning. Unfortunately, urinary tract endometriosis may also coexist with endometriosis in other areas such as the bowel and may also require a Colorectal surgeon’s involvement.
The management options for endometriosis in the urinary tract depends on symptoms and the result of investigations. The affected person must be at the centre of any decision making about their care and are fully informed of all their options and the benefits and risks of each option provided. They must meet and spend time with any other specialist that may become involved in their future surgical care.
The management of endometriosis can be divided into medical and surgical treatments. Medical treatments have been covered in previous Endometriosis Australia blogs. If people are not responding to medical treatments, they may elect to pursue surgical therapies. If a ureter or kidney function is being affected, then surgery may be the only feasible option.
Laparoscopic (keyhole) surgery under general anaesthetic has become the mainstay of surgical techniques used to treat all forms of pelvic and extra pelvic endometriosis. In most cases, an experienced and trained endometriosis specialist will excise superficial peritoneal endometriosis on the bladder and over the ureter. For deeper disease around the ureter, careful dissection to excise endometriosis from around the other structures, including blood vessels and pelvic nerves, must be performed. If the endometriosis is compressing or obstructing a ureter, a urology surgeon may become involved to unblock the ureter or even cut the ureter and reimplant the ureter into the bladder clear of any disease. It is prudent that the original disease causing the obstruction of the ureter is resected.
Deep disease that is growing into the bladder muscle wall can be seen by passing a camera into the bladder. The deep disease may then be removed from the bladder wall itself (Image 6). If the inside of the bladder is opened, the hole is repaired with dissolving sutures (Image 7). The patient will require a catheter in the bladder for up to ten days to allow the bladder wall to heal. The patient can go home usually after a few days and is given a bag that attaches to their leg to collect their urine. In the more severe urinary tract endometriosis cases, a urologist may place stents that stay in place for several weeks to allow the ureter to heal. In very rare cases, a kidney may need to be removed by a urologist because of long term damage from endometriosis.
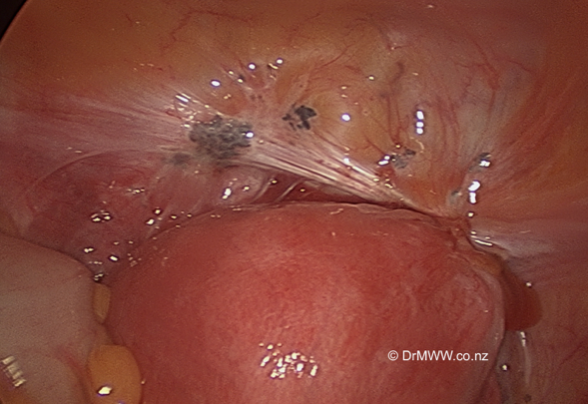
Image 6: Deep infiltrating bladder endometriosis seen from a laparoscopic view
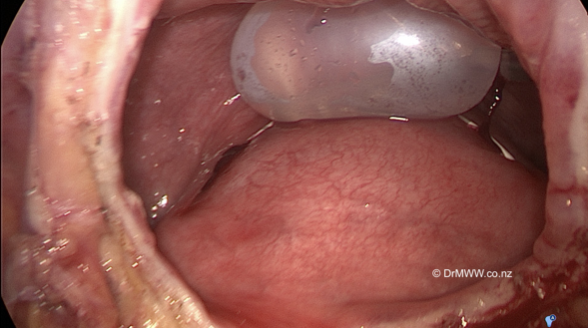
Image 7: The inside of the bladder (with inflated catheter balloon) after resection of the deep endometriosis. The bladder defect will be repaired with sutures.
People who have had complete excision of deep endometriosis from their bladder and/or from around their ureters do very well, as the relief of their pain, and other symptoms can be quite significant. We know that up to 50% of people can have a recurrence of their pain symptoms at some point in time after surgery. Medical treatments can be useful after surgery to reduce recurrence and to help control pain. Your GP and Specialist can help you develop a multidisciplinary team if required to help manage any recurrent pain and maintain a lifestyle that meets your needs and desires. Recurrent surgical procedures should be avoided without good reason, as the benefits reduce with each subsequent operation.
People diagnosed with endometriosis are encouraged to become well informed about their condition, so they can navigate the sometimes-complex labyrinth that a life with endometriosis and pelvic pain can become.
Written by,
Dr Michael Wynn-Williams
March 2021
Auckland, New Zealand
*this blog has been written in gender-inclusive language

