Management and Treatment
Overview of Endometriosis Treatment Options
Endometriosis treatment often combines several approaches tailored to your symptoms and lifestyle. Common treatment options for endometriosis include:
- Medicines
- Surgery
- Other therapies
Finding the right approach to managing endometriosis and endometriosis treatment may involve a combination of these strategies with guidance from your healthcare team.
Medical endometriosis treatments
Choosing the Right Medical Endometriosis Treatment
Medical endometriosis treatments can be broadly grouped into hormonal and non-hormonal options.
Hormonal treatments for endometriosis
Common hormone treatments include:
- the oral contraceptive pill
- progestogens (one of the two main female hormones), which can be taken as tablets, an injection that lasts 3 months, a small rod placed under the skin (implant), or an intrauterine system (like an IUD).
Talk to your doctor about the different treatments. There are advantages and disadvantages for all treatment options. You may have a combination of treatments and it make some time to find the right combination for you.
There are several other hormonal treatments that can be used for short periods. These are powerful medicines and can cause significant side effects if used for long periods.
Side effects of hormone treatments can include:
- Breakthrough bleeding or spotting
- Bloating
- Nausea
- Weight gain
- Mood changes or depression
- Changes in skin (oily or spotty skin)
- Higher blood pressure.
Non-hormonal medications for pain relief
These can help with pain but will not reduce the amount of endometriosis in your body. They may be used on their own or in combination with other treatments.
Common options include:
- paracetamol
- non-steroidal anti-inflammatory drugs (NSAIDs)
- strong pain medicines.
Surgical endometriosis treatment options
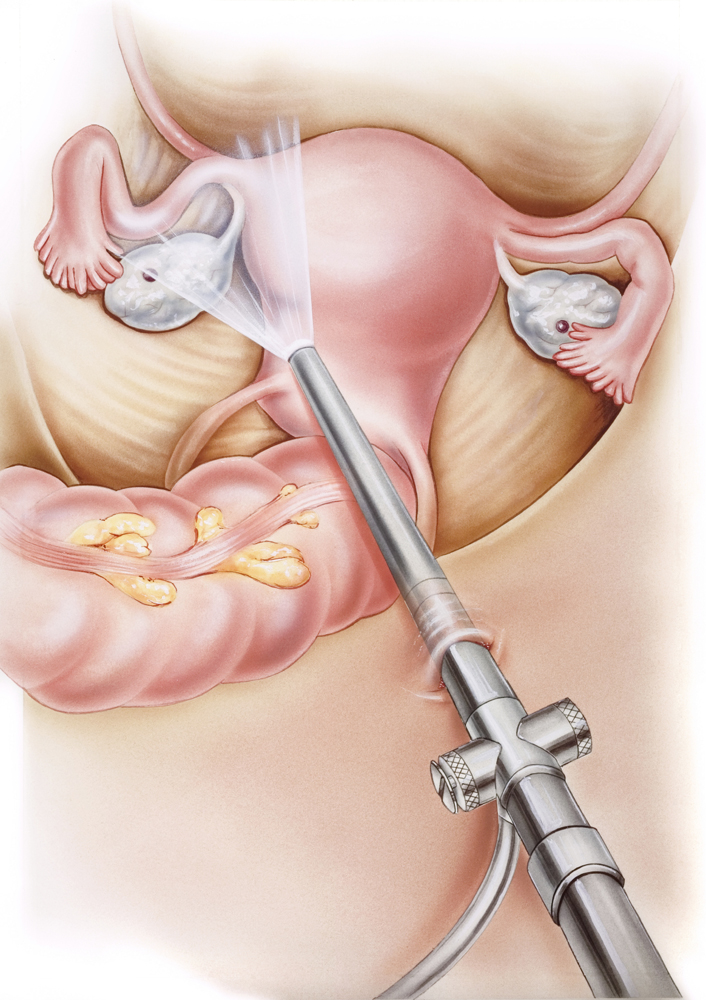
Surgery for endometriosis includes laparoscopy or laparotomy.
Your doctor will talk to you about the most suitable surgery, as well as the risks of each procedure and any possible complications. You will be asked to sign a consent form before your procedure.
Laparoscopy – Also called keyhole surgery, this is the most common type of surgery for endometriosis. It causes less scarring, less pain, less time in hospital. It allows the surgeon to better see the areas where endometriosis is growing and small bleeding points can be more easily seen. Usually your doctor will inform you of the chances of this prior to your surgery.
Laparotomy – Also known as open surgery, this is more commonly used for severe endometriosis. Laparotomy means the surgery is performed through the abdomen, and a large cut is made along the bikini line to the pubic area. Occasionally, the cut is made from the belly button the pubic area instead.
Very occasionally, a laparotomy is needed to finish keyhole surgery or if a complication occurs during the operation.
Side effects of surgery
As with any surgery, risks include damage to other organs such as the bladder, bowel, ureters (the tubes that lead from the kidneys to the bladder) or the large blood vessels.
Damage to other organs would be mean more surgery – either by laparoscopy (key hole surgery) or a laparotomy (large cut in the abdomen).
How complementary therapies support endometriosis treatment
Using allied health professionals for treatment
Other types of therapies can manage the symptoms of endometriosis. Some people find it helpful seeing professionals such as:
- physiotherapists
- acupuncturists
- herbalists
- dietitians
- homeopaths
- psychologists
It’s important to talk to your doctor before starting any treatments, especially if you are having surgery, as some therapies can affect surgery.
Physiotherapist: A physiotherapist who specialises in pelvic health can help with bladder, bowel or pelvic muscle-related pain. They are trained to deal with these specific issues. Ask your doctor if they can recommend a physiotherapist in your local area.
Clinical psychologist: They can help with managing the emotional impact of living with chronic pain. They can teach you coping strategies for pain, stress, anxiety, depression, mood changes and changes to relationships.
Understanding pain
There are two parts to pain:
- the cause, such as endometriosis
- the brain’s response to the pain.
Treating endometriosis with surgery or medicine may relieve symptoms. However, if the pain continues this does not mean that the endometriosis has come back – it could be the way the brain is processing the pain.
While pain medicines can provide relief this may only be short term. Learning ways to manage ongoing (chronic) pain can help.
What is the best treatment for endometriosis?
There is no single ‘best treatment’ for endometriosis as everyone is different. It’s important to know about the different treatments options, including their benefits, side effects and complications. You may need a combination of treatments to help manage the symptoms of endometriosis.
What to expect after treatment
Most treatments help manage endometriosis symptoms, but they may not reduce pain completely. Some people will have pain even without endometriosis, and pain or infertility can have other causes.
- For most people, treatments can reduce symptoms by 50-70%.
- Some people may not get any relief from any treatment.
- In this case, other tests and ways to manage symptoms may be necessary.
- Symptoms can come back (recur) in about 1 in 3 people. This may happen months or years after treatment. It’s hard to know who will respond to treatment.
For people with severe endometriosis (stage 4), endometriosis may come back in about 70% of cases. However, many people can have a good quality of life and become pregnant after treatment.
What are the risks of treatment?
Medical treatments can be associated with side effects such as:
- spot bleeding
- breakthrough bleeding
- bloating
- nausea
- weight gain
- depression
- skin changes (oily or spotty skin)
- elevation in blood pressure.
For surgery, there are risks associated with the area being operated in, like damage to other organs such as the bladder, bowel, ureters (the tubes that lead from the kidneys to the bladder) or the large blood vessels. Damage to other organs would require repair usually by further surgery that may be done by laparoscopy or may require a laparotomy (large cut in the abdomen) to complete.
There are no known complications from seeing a psychologist or a physiotherapist. There can be side effects and complications from acupuncture, herbalism and other complementary medicines. You should ask your health care professional about risks associated with a treatment or procedure before commencing that treatment or having a procedure.
Medical information disclaimer
Endometriosis Australia’s information about the diseases, treatments and general matters has been written and edited by Endometriosis Australia’s volunteers. Endometriosis Australia makes every effort to ensure the information provided is as up-to-date and accurate as possible, however does not accept liability for misinterpreted or incorrect information.
It is also not the intention of Endometriosis Australia to recommend any particular form of treatment. At all times you need to discuss the information you find on this website, or any other source, with your doctors or health team, given your unique situation and status.
