The human microbiome project (HMP) was first discussed in 2007 where it described humans as “Supra-organisms,” – a combination of human cells and microbial cells that include bacteria, viruses and fungi all living together (on and in the human!) It is notable that the number of microbial cells vastly outweigh the number of human cells by a ratio of about 10:1. That means for every human cell, there are 10 microbial cells on and in our bodies, but their small size means that the total weight of all of those cells is about 1-3%. So, for a woman weighing 60kg, this would be about 600g-1.8kg of microbes! (1)
About the microbiome
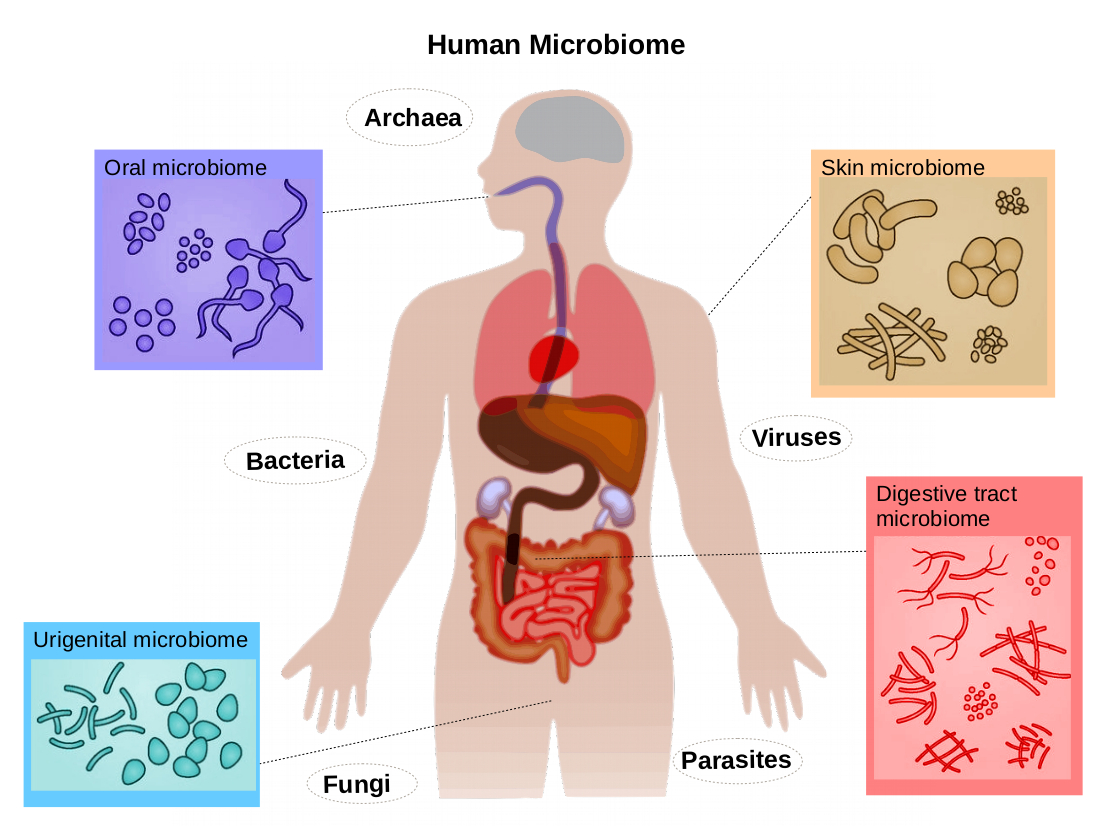
Microbes have always been a part of human lives, living and evolving alongside us and although it is not yet clear whether nature or nurture played the most important role in the development of a human microbiome, it is probable that both the environment in which both humans and microbes live and the mutual benefits that are gained from the two coexisting that allow this to continue today (2). There has been a spotlight on what the impact microbes which inhabit our bodies have on our health, and likewise on disease states (3). Research in this area is still very early, and facing several challenges, since the huge number of cells (remember the 10:1 ratio) mean that simply identifying them all is difficult and then working out which ones may contribute to the health or disease states is complex (to say the very least). However, it is important to keep exploring possible connections of all of the relationships of the microbiome to help direct future research and improve the health of people with endometriosis.
This article will open up a brief discussion around the current understanding and theories of the role of the microbiome in relation to endometriosis.
The microbiome is defined as the genetic material of all microorganisms living in and on our bodies (4). It seems that as humans have evolved, so to has the microbiome – possibly related to our living conditions, diet and social habits. So as human populations passed through three stages of subsistence:
- Foraging
- Rural farming
- Industrialised western life
our microbiomes have become very different (2).
There has been much discussion around whether a particular microbiome profile matches a ‘healthy’ human. Current research suggests that rather than being a ‘healthy’ profile that every human follows, each individual person has a unique core collection of microbes which is specific to them and fairly stable. So we could consider this as our ‘microbial fingerprint’ and this should give you some indication as to why it makes it difficult to study the microbiome. It is thought that any major variation from that core collection may affect an individual’s risk for disease (4).
The female reproductive system has been shown to be the home for distinct microbial communities, with differences in the types of cells that affect the skin at the vulva, along the vagina, and into the cervix and organs. In the vagina, the most common microbes are the lactobacillus species (5). These ‘friendly’ bacteria seem to work together with various different human cells and can influence important body functions such as:
- Keeping an eye out for harmful microbes (5).
- Keeping our hormones in balance (6).
- Maintaining our metabolic functions (6).
When it comes to women with endometriosis, researchers are starting to investigate a “bacterial contamination hypothesis” (7). Research from Japan have collected information from a number of studies and suggest that chemicals released from the presence of large numbers of bacteria such as E-coli in the vagina (which are normally present in the bowel) may drive an inflammatory response. This in turn may alter the immune function in the pelvis that is so often seen in endometriosis (8).
Other specific microbial families that may contribute to endometriosis are an increased number of Proteobacteria, Enterobacteriaceae, and Streptococcus in addition to the E coli (9,10). It is not just an increase in the number of microbes that could lead to problems, with a decrease in the normally abundant vaginal lactobacilli also noted to be potentially problematic and called a disturbed or dysbiotic microbiome (11). It has also been suggested in early research that people with later stage (advanced) endometriosis may have specific microbe variations in their reproductive tract (4).
What hasn’t been established yet however, is which situation occurs first. Is it the endometriosis that causes changes in the microbes in and on our body? Or is it that alterations in the microbiome contributes to the formation of or progression of endometriosis? We also don’t have standards to compare what is normal (like we do for say your iron level or the amount of sodium in your body), so ‘microbiome testing’ should only be taking place inside a specific research program at this current time so we can improve our knowledge in this area. Others issues around research are consideration of life style habits such as diet and nutrition on the bacteria present in your body, the effect of any underlying pre-exisiting diseases that may change the microbiome (such as inflammatory bowel disease) or obesity (12). How we find, count and compare the microbiome is not yet uniform across all research sites, and growing some of the bacteria is tricky, which may alter results (13). All of these factors mean we are just at the beginning of the research program for the microbiome and endometriosis. It also means that antibacterials, antivirals and antifungals should not be considered as a ‘treatment’ for endometriosis based on any measurement of the organisms on our bodies. It is also important that specific infections such as urinary tract infections, sexually transmitted infections or skin infections are appropriately identified, and treated since this may be medically important.
Summary
We do know that endometriosis is an inflammatory disease being driven by changes in hormonal levels – with oestrogen the principal driver. This inflammatory process is encouraged by various proteins that are released by specific types of immune cells and these may alter function in endometriosis patients (10). In a dysbiotic microbiome, bacteria are known to produce inflammatory compounds, and these have some scientific evidence to show that they can affect circulating oestrogen levels (14). This is the proposed theory for how the microbiome may have a major impact on endometriosis.
Much more work needs to be done before we can establish a clear relationship between the microbiome and the development and progression of endometriosis. Very importantly, there is a need to characterise the “core” make-up of the healthy microbiome along the whole reproductive tract and to establish both the ways that we can detect, categorise and treat the microbiome to make it work to our benefit.
Tracy Gaibisso
MRMed. GradCertWellness. AdvDipNat. DipNut. DRM. MATMS
Jason Abbott
B Med (Hons) FRANZCOG FRCOG PhD
References
1) Turnbaugh PJ., Ley RE., Hamady M., Fraser-Liggett CM., Knight R., Gordon JI. (2007). The human microbiome project. Nature. Oct 18;449(7164):804-10.
2) Gupta, V. K., Paul, S., & Dutta, C. (2017). Geography, Ethnicity or Subsistence-Specific Variations in Human Microbiome Composition and Diversity. Frontiers in microbiology, 8, 1162. https://doi.org/10.3389/fmicb.2017.01162
3) Zhang YJ., Li S, Gan RY., Zhou T., Xu DP., Li HB. (2015) Impacts of gut bacteria on human health and diseases. Int J Mol Sci;16:7493-519
4) Ata, B., Yildiz, S., Turkgeldi, E., Brocal, V. P., Dinleyici, E. C., Moya, A., & Urman, B. (2019). The Endobiota Study: Comparison of Vaginal, Cervical and Gut Microbiota Between Women with Stage 3/4 Endometriosis and Healthy Controls. Scientific reports, 9(1), 2204. https://doi.org/10.1038/s41598-019-39700-6
5) Agostinis, C., Mangogna, A., Bossi, F., Ricci, G., Kishore, U., & Bulla, R. (2019). Uterine Immunity and Microbiota: A Shifting Paradigm. Frontiers in immunology, 10, 2387. https://doi.org/10.3389/fimmu.2019.02387
6) Qi, X., Yun, C., Pang, Y., & Qiao, J. (2021). The impact of the gut microbiota on the reproductive and metabolic endocrine system. Gut microbes, 13(1), 1–21. https://doi.org/10.1080/19490976.2021.1894070
7). Khan, K. N., Fujishita, A., Hiraki, K., Kitajima, M., Nakashima, M., Fushiki, S., & Kitawaki, J. (2018). Bacterial contamination hypothesis: a new concept in endometriosis. Reproductive medicine and biology, 17(2), 125–133. https://doi.org/10.1002/rmb2.12083
8). Wei, W., Zhang, X., Tang, H., Zeng, L., & Wu, R. (2020). Microbiota composition and distribution along the female reproductive tract of women with endometriosis. Annals of clinical microbiology and antimicrobials, 19(1), 15. https://doi.org/10.1186/s12941-020-00356-0
9) Akiyama, K., Nishioka, K., Khan, KN., et al.(2019) Molecular detection of microbial colonization in cervical mucus of women with and without endometriosis. Am J Reprod Immunol. 82:e13147. https://doi.org/10.1111/aji.13147
10) Leonardi, M., Hicks, C., El-Assaad, F., El-Omar, E., & Condous, G. (2020). Endometriosis and the microbiome: a systematic review. BJOG : an international journal of obstetrics and gynaecology, 127(2), 239–249. https://doi.org/10.1111/1471-0528.15916
11) Jiang, I., Yong, P., Allaire, C., & Bedaiwy, MA., (2021) JInt. J. Mol. Sci. 22, 5644. https://doi.org/10.3390/ijms22115644 https://www.mdpi.com/journal/ijms
12) Al-Nasiry, S., Ambrosino, E., Schlaepfer, M., Morré, S. A., Wieten, L., Voncken, J. W., Spinelli, M., Mueller, M., & Kramer, B. W. (2020). The Interplay Between Reproductive Tract Microbiota and Immunological System in Human Reproduction. Frontiers in immunology, 11, 378. https://doi.org/10.3389/fimmu.2020.00378
13) Jason, M., Franasiak, M.D., & Scott, R.T. (2015). Microbiome in human reproduction. Fertil Steril!;104:1341–3. https://dx.doi.org/10.1016/j.fertnstert.2015.10.021
14) Ervin, S. M., Li, H., Lim, L., Roberts, L. R., Liang, X., Mani, S., & Redinbo, M. R. (2019). Gut microbial β-glucuronidases reactivate estrogens as components of the estrobolome that reactivate estrogens. The Journal of biological chemistry, 294(49), 18586–18599. https://doi.org/10.1074/jbc.RA119.010950
Written by,
Tracy Gaibisso & Prof Jason Abbott