By Dr Sofie Piessens – Endometriosis Australia’s Clinical Advisory Committee
(Content Warning: Some may find the educational images provided graphic.)
The ability to diagnose deep infiltrating endometriosis with transvaginal ultrasound has improved dramatically around the world since 2009.
What can the ultrasound diagnose?
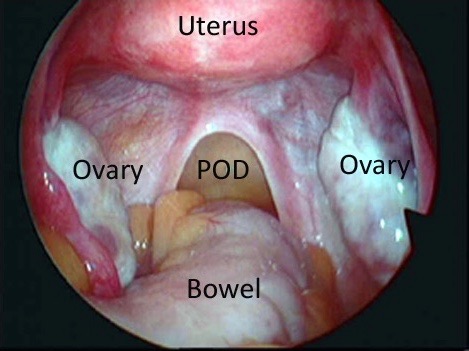
Endometriosis is defined as the presence of tissue similar to that of the lining of the uterus (endometrium) outside of the uterus, most commonly on and below the ovaries, and deep in the pelvis behind the uterus, called the Pouch of Douglas. Here, the endometriosis grows on the ligaments behind the uterus and on the vagina and rectum. It also may grow on the bladder, appendix, and even sometimes in the upper abdomen or in the abdominal wall in the scars of a laparoscopy or caesarean delivery.
There are many presentations of endometriosis which may be identified by the surgeon at laparoscopy.
A distinction is made between superficial lesions and deep infiltrating endometriosis.
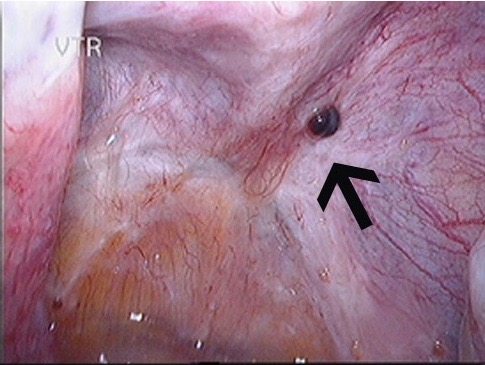
In the majority of women with endometriosis, the endometriosis found in the pelvis has only implanted superficially. Superficial lesions of endometriosis can never be diagnosed on ultrasound as they have no real mass, only colour, which cannot be detected with ultrasound. These lesions can cause as much pain as some deep infiltrating lesions but they can only be seen on laparoscopy. They may be removed during a laparoscopy and special preoperative measures are rarely required.
The image on the left shows a normal pelvis while the one on the right shows superficial endometriosis deposits.
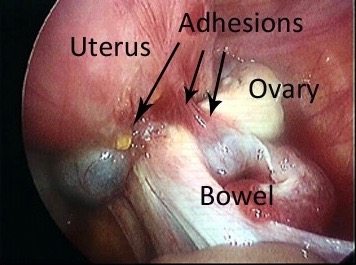
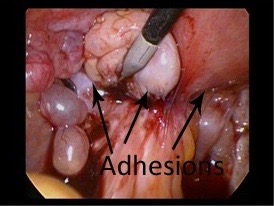
In about 20% of women with endometriosis, the endometriosis will not just superficially implant in the pelvis, but it will infiltrate into pelvic structures, mainly into bowel, bladder, the vagina and ligaments behind the uterus (uterosacral ligaments). This form of the disease is called deep infiltrating endometriosis (DIE). Deep infiltrating endometriosis causes usually more destruction of the normal anatomy and is generally significantly more difficult to remove. Because lesions of endometriosis infiltrate into ligaments, vagina, bowel and bladder, adhesions can occur between organs such as the bowel and the uterus or the uterus and the ovaries.
Both images below show deep infiltrating endometriosis with significant adhesions. Organs are stuck together.
Ultrasound can detect deep infiltrating endometriosis with a high degree of accuracy.
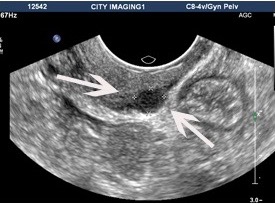
The larger the lesion, the easier it is to see on ultrasound, but in the hands of experienced imaging specialists lesions of only a few millimetres may be diagnosed. Endometriosis lesions on ultrasound look darker (seen as blacker) on ultrasound.
The left image shows a small lesion on the back of the vagina, causing pain with sexual intercourse. The right image shows a large bowel lesion, which seems very easy to see, but unless the bowel is inspected, it is not noticed on routine pelvic ultrasound.
Why is the preoperative diagnosis of deep infiltrating endometriosis important?
The gold standard of endometriosis diagnosis is laparoscopy as laparoscopy can diagnose all forms of endometriosis, something no other test can. It is however important to have a detailed ultrasound prior to considering a laparoscopy to look for deep infiltrating endometriosis. Often when deep infiltrating endometriosis is unexpectedly found at laparoscopy, the removal of endometriosis cannot be completed as special preparation is required to allow removal of such lesions. The woman may need specific bowel preparation, and often it is preferable to have a colorectal surgeon present at the surgery since a section of bowel may need to be removed. The preoperative diagnosis of deep infiltrating endometriosis may give a first explanation for symptoms but more importantly, it gives an indication of the extent of the disease, it provides patients with the time to think about the extent of the surgery they are prepared to submit to, and gives the surgeons an idea of what they will find during the surgery so they can prepare better for the operation and advise patients better regarding other treatment options available. The necessary preparations can be made prior to starting the first laparoscopy and repeat surgery can be avoided. Ultrasound will not detect superficial lesions so in case of a normal ultrasound a laparoscopy may still indicate when there are significant symptoms.
How is the ultrasound performed?
A normal ultrasound is performed using a transvaginal probe (a thin instrument about the thickness of your thumb that is gently placed into the vagina to allow for better vision of the pelvic structures). The scan may be done through the rectum, but is rarely performed in Australia, since women find this more uncomfortable than the transvaginal method. The ultrasound usually takes 30 minutes. Because endometriosis can infiltrate the bowel, the doctor or sonographer who does the ultrasound will carefully look at the bowel during the transvaginal ultrasound. When the rectum is empty, the views of the bowel are generally better since faeces and gas in the bowel cause shadows on ultrasound. For this reason, some doctors prefer you to take a mild bowel preparation prior to the ultrasound when you have had a past history of severe endometriosis or when you have significant bowel pain during your periods. This consists of a mild laxative the night before the ultrasound and an enema an hour before the ultrasound. If you don’t have a proven history of significant endometriosis, or no significant bowel symptoms or signs on examination, it is probably not necessary to take bowel preparation and a regular scan could be performed.
Can the ultrasound be performed by any imaging technician?
Hopefully, in the future, anyone who performs a gynaecological ultrasound will look for deep infiltrating endometriosis but that is unfortunately not yet the case. A ‘normal’ gynaecological ultrasound traditionally only involved looking at the uterus and ovaries. Unless endometriosis forms cysts on the ovaries (endometriomas) it is therefore not picked up with a traditional gynaecological ultrasound. Looking for endometriosis involves looking not just at the uterus and ovaries but also at the bladder, the ligaments behind the uterus, the vaginal wall and the bowel. It also involves assessing the mobility of the ovaries and checking whether there is sliding between the bowel and the uterus. This is not difficult to learn and does not feel any different for the person undergoing the ultrasound. It does however involve a change from current practice and it always takes time for such a change to take place. A number of Australian sonologists and sonographers have developed an expertise in the diagnosis of deep infiltrating endometriosis and are striving to improve the skill of most imaging specialists through workshops and education. This will hopefully lead to the examination being available to all Australian women with symptoms of endometriosis. Women and referring doctors can initiate change by expecting an assessment for endometriosis to be performed as part of a routine gynaecological condition which may in turn stimulate imaging specialists to learn and include this assessment in every ultrasound they perform, particularly when performing an ultrasound for symptoms consistent with endometriosis.
By Dr Sofie Piessens