By Associate Professor Louise Hull – Endometriosis Australia’s Clinical Advisory Member
Last updated: 13 November 2025
 Endometriosis is where the cells similar to the lining of the womb grows at an unusual site like in the pelvic cavity. Although in the past it was only though to affect older women, we now know that it is common to get endometriosis as a teen or young woman and there is a lot that can be done to help.
Endometriosis is where the cells similar to the lining of the womb grows at an unusual site like in the pelvic cavity. Although in the past it was only though to affect older women, we now know that it is common to get endometriosis as a teen or young woman and there is a lot that can be done to help.
I thought the best way of blogging about adolescent endometriosis was to answer a lot of the questions that I get asked in my adolescent gynaecology clinic.
Do women with endometriosis get symptoms in their teens?
Most women with endometriosis say that their period pain started in their teens or early 20s, commonly around the time they started having periods. An American endometriosis registry found that 38% of women started experiencing period pain before 15 years of age (1).
How common is period pain in adolescents?
It is common. An Australian study in Canberra of 1000 schoolgirls aged 16-18 found that 93% had painful periods. Of these 21% had severe period pain and 26% missed school for period pain or a mix of period symptoms (2).
What is the difference between ‘normal’ period pain and pain that needs further investigating?
Mild discomfort on the first 1-2 days of a period is common and reasonable, particularly if painkillers are effective.
A doctor should be consulted if the pain:
Causes distress or inability to go to school or do others activities (sport, social events etc)
Occurs outside the first 2 days of the period
Doesn’t get better when treatments like the pill or painkillers are taken
What other symptoms can teenagers get?
There are several reasons for pelvic pain from endometriosis. Endometriosis responds to reproductive hormones like the lining of the womb. When women get their period, the endometriosis tissue can breakdown and irritate the pelvic environment causing pain. The pelvic muscles can then respond by contracting and having muscle spasms (which causes pain). After a while the brain gets sensitised to the pain (central sensitisation) and headaches and fatigue can occur. All these pain symptoms impact on general wellbeing and can reduce energy levels as well as mood. Because of this the best approach to endometriosis is to use pain management methods that address all these aspects of pain.
Some other symptoms women with endometriosis can get include:
- Heavy periods
- Bloating
- Lower back pain
- Chronic pain throughout the cycle
- Pelvic muscle spasm
- An irritable bowel
- A painful overactive bladder
- Headaches
- Fatigue
If adolescents have pain that doesn’t respond to pain medications or the pill, how often do they have endometriosis?
Between 67-73% will have endometriosis when diagnostic surgery is performed (3,4).
Which teens are at risk of endometriosis?
Endometriosis has a tendency to run in families, so young women with relatives with endometriosis (mothers, sisters and aunts) have a higher chance of having endometriosis (5).
Adolescents who start having periods earlier (6) and have a lower BMI (7) have a higher risk of having endometriosis.
Very rarely, some women are born with a reproductive tract shaped in a way that blocks normal menstrual flow so more endometrial fluid and tissue flows back into the pelvic cavity where it becomes endometriosis. About 50% of teenagers with wombs shaped this way have endometriosis (8).
Most girls and women with endometriosis have a normally shaped uterus.
How is endometriosis diagnosed in adolescents?
Ultrasounds and MRI scanners detect endometriosis cysts on the ovaries quite well (8), but these are rare in adolescents so may not detect endometriosis even if it is present in young women.
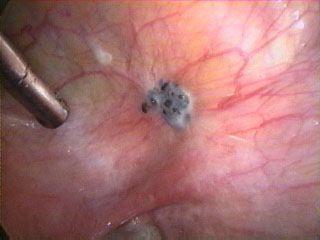
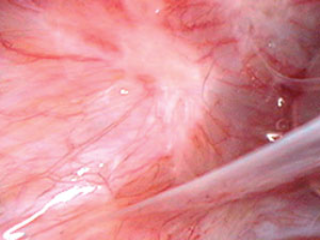
Younger women tend to have smaller lesions that are clear or white or red (as opposed to dark/brown lesion seen in older women –see below) on the surface of the pelvic cavity (peritoneum) (9). These lesions can only be detected when they are seen by a surgeon undertaking a diagnostic laparoscopy (keyhole surgery using a small telescope through the belly button). As these lesions can be subtle it is important to engage an experienced surgeon to make the diagnosis.
How well does surgery treat endometriosis symptoms in adolescents?
Surgery is best regarded as a way of diagnosing endometriosis and one method to manage pain (rather than cure it). Even when all the endometriosis has been removed, there is less pain and endometriosis is less likely to recur if periods are suppressed. The best plan is to have as few and as light periods as possible. This might mean taking the pill to minimise periods, using a tablet like dienogest daily, or having a Mirena Coil inserted. If periods are heavy more than one of these treatments may be required. Gynaecologists are the best people to ask about surgery for endometriosis and pain management before and after the surgery.
What can adolescents with significant period pain do to manage their symptoms?
Keeping active rather than resting all day will reduce the pelvic muscle spasm that is so common in women with endometriosis and pelvic pain. Girls who spend a lot of time resting can find their pain worsens. Gentle exercise such as walking or stretching will help.
Good women’s health physiotherapists that understand it is important for women with pelvic pain to relax rather than tighten their pelvic floor, can also provide helpful advice and support.
Young women with bowel symptoms (bloating, pain high in the abdomen or on the left side and pain that is relieved by passing a bowel motion) can often find relief by improving their diet and avoiding constipation. Drinking plenty of water, eating diets that contain lots of fibre or considering diets such as the FODMAP diet with a low content of fermenting sugars (See the Monash University website https://www.med.monash.edu/cecs/gastro/fodmap/) can be useful. Every person responds differently to diet and this does need to be personalised. Dieticians can be a great source of support to improve pain symptoms through diet.
Finding enjoyable absorbing activities that distract from pain symptoms is another way that teens can improve symptoms. Handcrafts, Art, looking after animals etc can bring some relief from focusing on pain symptoms and improve mood symptoms. Mindfulness meditations can also focus the mind away from pain symptoms and can help in pain management.
Having a hot bath or using a hot water bottle can help relax the pelvic floor and improve pain symptoms.
Acupuncture and alternative therapies can improve pain symptoms for some young women and are worth exploring.
What can parents do to help their teen manage endometriosis pain?
Get good information about pelvic pain
Recognise the effects of pain on your adolescent’s thoughts and emotions
Help your daughter develop a support team (this may include general practitioners, gynaecologists, physiotherapists, pain management specialists, dieticians, personal trainers, and counsellors as well as relations, friends, teachers and the school nurse)
Encourage your adolescent to go to school and maintain their social network and lead as normal a life as possible.
Shift the focus away from pain
Help your adolescent develop a plan to manage a bad pain day
What other treatments can doctors prescribe for teens with endometriosis?
Non-steroidal anti-inflammatory medications (Naprosyn or Ibuprofen) are commonly used. They are best taken before the period pain becomes severe. When the pain starts, 2 tablets are taken straight away then 1 further tablet taken no more than 3 times a day while the pain lasts. It is important to take them only while the pain is severe, as they can cause stomach ulcers if taken over too long a period of time.
Sometimes medications that treat the nerves response to pain (such as amitriptyline or duloxetine) can be useful in managing endometriosis symptoms. Usually small doses are taken daily at night as they can cause drowsiness and they take a few weeks to work. Opiates should be avoided as although they work for short term pain (for instance just after surgery) in the long term they can make pain worse. A pain specialist is the best person to prescribe these medications.
Tablets such as the contraceptive pill, dinogest or norethisterone have the hormone progesterone in them. Progesterone suppresses the growth of endometriosis which can help with pain management. The pill can also be taken in ways that lets teens skip periods (and the pain that goes with them) reducing the number of painful periods in a year.
Progesterone is also in Implanon which is a small insert that can be placed under the skin in the upper arm. This can make periods lighter or suppress them and can help with pain management for some adolescents with endometriosis.
The Mirena intrauterine contraceptive device also contains progesterone. This device can be placed in the womb where is acts locally to reduce the growth of the womb lining and any nearby endometriosis lesions. Its most common use in adolescents is for period suppression and treatment of endometriosis pain. Young women considering surgery for endometriosis can have this placed during surgery while they are asleep.
General practitioners, gynaecologists and pain specialists can provide more information about medications that help manage endometriosis.
Do adolescents with endometriosis have to worry about their future fertility?
Although many women with endometriosis do conceive naturally and easily, women with endometriosis are more likely to have difficulty conceiving. This is mainly due to the effect of inflammation in the pelvis which can cause metabolic stress for eggs in this environment. Because of this, women with endometriosis can have fewer eggs and surgery (particularly surgery that removes endometriosis ovarian cysts) can reduce eggs numbers as well.
The egg timer test (blood tests and scans) can provide information about how many eggs are in the ovaries, although this test works better for women in their 20s and above. Egg freezing technology has improved and it is possible for young women with endometriosis to freeze eggs if their egg numbers are low or if they plan to have surgery that involves the ovaries, so they can use these eggs to conceive later in life. General practitioners, gynaecologists and fertility doctors can provide more information about preserving fertility.
References
1. Ballweg, ML. Big picture of endometriosis helps provide guidance on approach to teens: comparative historical data show endo starting younger, is more severe. J Pediatr Adolesc Gynecol 2003; 16 (3 Suppl): S21-S26.
2. Parker MA, Sneddon AE, Arbon P. The menstrual disorders of teenagers (MDOT) study: determining typical menstrual patterns and menstrual disturbance in a large population-based study of Australian teenagers. Br J Obstet Gynaecol 2010; 117(2): 185-192.
3. Reese KA, Reddy S, Rock JA. Endometriosis in an adolescent population: the Emory experience. J Pediatr Adolesc Gynecol 1996; 10: 125-128.
4. Laufer MR, Goietein L, Bush M, Cranmer DW, Emans SJ. Prevalence of endometriosis in adolescent girls with chronic pelvic pain not responding to conventional therapy. J Pediatr Adolesc Gynecol 1997; 10: 199-202.
5. Stefansson H, Geirsson RT, Steinthorsdottir V, Jonsson H, Manolescu A, Kong A, Ingadottir G, J. Gulcher J, K. Stefansson K. Genetic factors contribute to the risk of developing endometriosis. Hum Reprod 2002; 17(3): 555-9.
6. Shah DK, Correia KF, Vitonis AF, Missmer SA. Body size and endometriosis: results from 20 years of follow-up within the Nurses’ Health Study II prospective cohort. Hum Reprod. 2013 Jul; 28(7): 1783-92.
7. Ugŭr M, Turan C, Mungan T, Kuşçu E, Senöz S, Ağiş HT, Gökmen O. Endometriosis in association with müllerian anomalies. Gynecol Obstet Invest. 1995; 40(4): 261-4.
8. Nisenblat V, Bossuyt PMM, Farquhar C, Johnson N, Hull ML. Imaging modalities for the non-invasive diagnosis of endometriosis. Cochrane Database of Systematic Reviews 2016, Issue 2. Art.No.: CD009591. DOI: 10.1002/14651858.CD009591.pub2
9. Redwine DB, Age-related evolution in the colour appearance of endometriosis. Fertil Steril 1987; 48 (6):1062-1063