What is pain science education? Pain science education aims to help people better understand what pain is, how it works, why we get it. When we better understand pain, we can find better ways to manage it.
What are the most important things to learn about pain for people with persistent (chronic) pelvic pain?
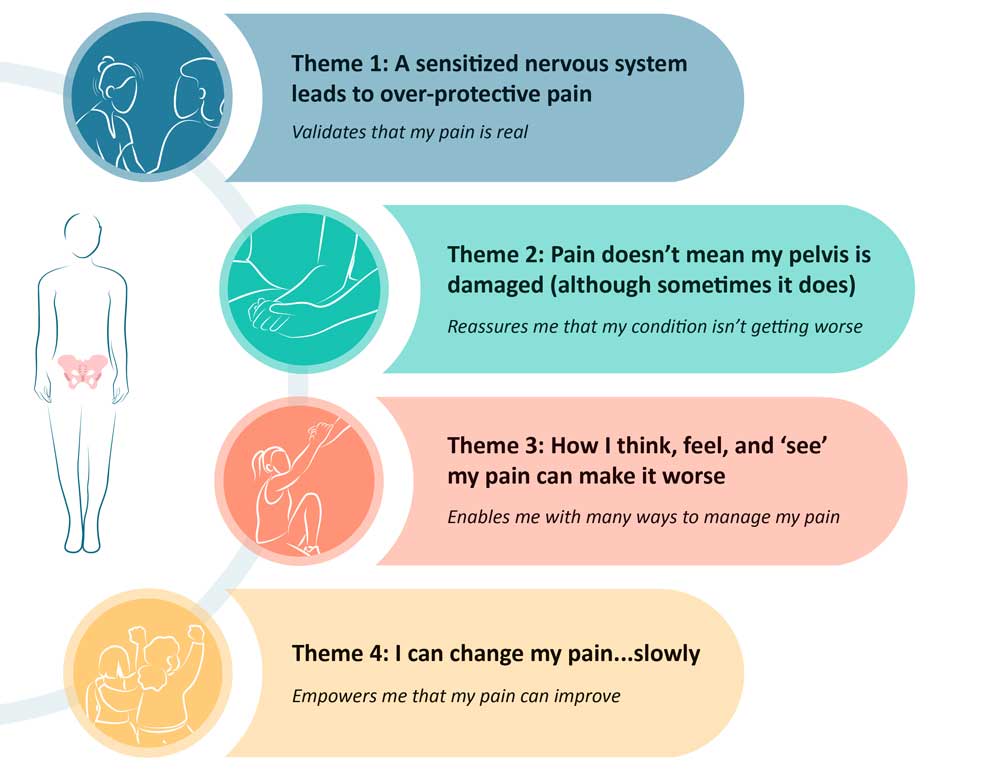
The four important concepts are:
1. A sensitised nervous system leads to over-protective pain
When we have pelvic pain that has been going on for a long time, our brain and nervous system becomes more sensitive and overprotective to different stimuli. When this happens, things can start to become more painful, or we get pain more frequently. Things that didn’t used to hurt can also start to become painful (like wearing tight clothing or eating particular foods).
Learning about how the brain and nervous system change with persistent pelvic pain was important because it provides validation that their pain is real. There are physical changes happening in our body that explain why pelvic pain gets worse over time. Pain is never ‘all in your head’. All pain is real, 100% of the time.
2. Pain doesn’t mean my pelvis is damaged (although sometimes it does)
Because our brain and nervous system become more sensitive with persistent pain, pain becomes less reliable at telling us what is going on in our pelvis. Some people with ‘mild’ endometriosis have really bad pain, whereas some people with ‘severe’ endometriosis have little to no pain at all.
Understanding that pain is more than what is going on in the pelvis was reassuring for people with endometriosis that if they did experience a pain flare, it did not mean that their endometriosis was getting worse. Pain can be influenced by many things – which we will discuss next!
3. How I think, feel, and ‘see’ my pain can make it worse
What is going on in the pelvis is one important part of the pelvic pain puzzle. However, pelvic pain can also be influenced by psychosocial factors. This includes things like worry and stress, our relationships with family, friends and colleagues, and stigma associated with pelvic pain.
When we better understand other factors that can influence pelvic pain, we can find better ways to manage it. If pelvic pain is worse during stressful times, doing stress management techniques or relaxation may benefit. If certain movements or activities are painful, gradually building up tolerance to exercise or pacing activities throughout the week can be helpful.
4. I can change my pain… slowly
The final thing that was important for people with pelvic pain to learn was that pain can change and get better over time. Just at the brain and nervous system changes to become more sensitive, they can change to become less sensitive, resulting in less pain. Unfortunately, this does take time. But working alongside a good team of healthcare professionals, pelvic pain can improve.
If you want to learn more about pain, speak to your healthcare professional. Pelvic health physiotherapists are particularly knowledgeable about pain and the pelvis!
Written by Amelia Mardon, PhD Candidate, Body in Mind Research Group, University of South Australia

